The “latent” period of postpartum recovery occurs from 6 weeks to 6 months after delivery but full postpartum recovery takes up to 2 years (that we are aware of in 2025). By that time, your hair should stop falling out. You should no longer have physical symptoms (like bladder leakage or Diastasis Recti). Your period may come back around the 6 month mark, but it could take up to 2 years for your hormones to re-balance. If you’ve had a C-section, you may feel more tired at the 6 month mark than those who had a vaginal delivery. Mentally, you may be getting more into a routine as your baby is sleeping more. Though, of course, it is important to address any lingering mental health concerns.
Weeks 1-2 Postpartum
Here at Recharged PT, we’ve talked extensively about what to expect prior to getting pregnant as well as the 1st, 2nd, and 3rd trimesters. Heck, we’ve even done a deep dive on the fourth trimester. But, sometimes, it can be helpful to get back to basics: what your recovery may look like after you give birth. Having a general timeline for postpartum recovery can be helpful - here are the first two weeks laid out for you.
Pregnancy Swelling!
We’re here today to talk about maybe one of the most common complaints seen during pregnancy and postpartum: swelling.
Swelling during pregnancy is usually pretty common in the lower extremities and feet. All the extra fluid that your body creates to help support a healthy baby can cause blood circulation to slow – and much of it accumulates in the legs and feet. Especially if you are up on your feet a lot!
Bladder Prolapse
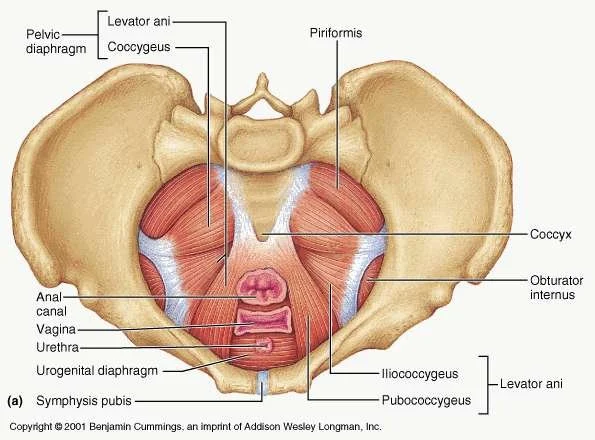
Cystocele (SIS-toe-seel) is when the bladder drops from its usual position and presses on the vaginal wall. A type of pelvic organ prolapse, cystocele or anterior vaginal prolapse, can occur if the pelvic floor muscles are weak, the organ is not in the correct spot in the pelvis in general (especially post child birth) or if there is too much pressure put on the pelvic floor. Common causes of a prolapsed bladder include repetitive stress over time (e.g., coughing, improper lifting) or during vaginal childbirth.
After Surgery- Post Op
Today we are talking about how to care for yourself after you have surgery- this could be anything from a C-Section to a knee replacement. The info contained here isn’t super specific but that doesn’t make it any less important!!
Having surgery and recovering from it can be a very challenging process physically, mentally, and emotionally. Whether you elect to have it done or the procedure is absolutely vital to your health and well-being, surgery is trauma to your body: it takes a toll.
Best Tools to use in Labor
Hi Everyone! Here are our favorite tools to use to assist with pain and hip movement during labor. The more you can handle the pain & the more movement your hips can do- the better and faster your labor will be!
We carry all of these things with us when we do Birth Support for our Mama’s!!
To find these on Amazon- just click on the photo!
Obturator Internus Pelvic Floor Pain
The Obturator Internus (OI) is a muscle that sits deep in the hip girdle, running from the front of the pubic bones and inserting onto the greater trochanter (the top bony part of the thigh bone). The OI is a deep hip stabilizer, which means it helps stabilize the head of the femur (thigh bone) to keep it in socket. This muscle is also responsible for external rotation – or rolling out– of the hip and thigh. Additionally, the OI shares a fascial connection to most, if not all, of the deep pelvic floor muscles. People with dysfunction of the Obturator Internus often complete of a deep groin, hip or back pain that won’t go away with regular stretching.
Pelvic Health, Pelvic Floor Rehab, Pelvic Floor Exercises, Pelvic Pain, Pain with Intercourse, Melbourne, FL, Postpartum, Postpartum Rehab, Pee Leakage, Dr. Paige, Dr. Laura, Recharged Performance Therapy
Stress Urinary Incontinence - Pee Leakage
One important thing to *note* here is that a lot of “Dr. Google” resources on SUI is that Kegels (tightening your PF muscles) will help with leakage by making the muscles stronger. But this is usually not the case!! The vast majority of people with pelvic floor dysfunction (and SUI) have have PF muscles that are too tight – NOT too loose. Because muscles need to be a certain length to work optimally, a muscle that is too loose OR too tight can be weak.
Pain with Intercourse
Vestibulodynia- Pain at the Opening of the Vagina
Vestibulodynia is chronic pain or discomfort that occurs around the opening to the vagina: the vestibule is where the lips of the vulva meet your vagina. It is a very sensitive part of your body and contains multiple glands to help with lubrication/discharge as well as the urethra. Pain may occur when the area is touched, during sex, when using a tampon or other certain movements like prolonged sitting. The area may even be chronically red and inflamed.
Abdominal Organ Mobilization
4th Trimester Part 2!
The 4th trimester also includes your baby’s adjustment into this crazy, colorful world! Dr. Antony Karp is credited with creating the concept of the 4th trimester. He posts that full-term babies are born three months too early relative to other mammals. This is possibly so that the head can fit through the birth canal. But, the flip side is that your baby’s nervous system is not yet fully developed – and has a hard time handling life outside a quiet, safe womb.
4th Trimester - part 1
A newly described phase of Pregnancy related care is being called the Fourth Trimester, lasting from birth until approximately 12 weeks postpartum.
This is a critical time for mommas that is often swept aside – there’s too much to do with a new baby, your house, all the family/friends trying to come over, and maybe your spouse… And if we are being honest, there not enough time or energy to do it all.
Superfoods for Your Pelvic Floor
An important subset of the physical component is what we eat: the type of fuel we give our bodies directly affects how we move through the world. Both physically and mentally.
Pelvic Floor Physical Therapy, Pelvic Floor Rehab, Pelvic Floor Melbourne FL, Dr. Paige, Recharged Performance Therapy, Recharged Pelvic Floor
G R A T I T U D E
Okay...guys! With Thanksgiving approaching, we often take the time to look at what we have been thankful for over the past year.
Research shows that developing a mindful gratitude ritual on a daily basis has tons of positive health benefits -- both mentally and physically.
Cultivating a sense of gratitude helps us feel connected to others as well as happier and healthier. It is more than just saying, “Oh, thank you!” when something good happens, but developing a grateful attitude on a consistent basis -- during the good days and the bad ones.
A feeling of gratitude has been linked to many benefits, including:
An improvement in overall physical health
Lower blood pressure
Better sleep
Better eating habits
An optimistic outlook on life
First, we want to be clear about the distinction between gratitude and “toxic positivity.” This is a term that has been floating around a lot recently -- and can sometimes be confused with gratitude. Taken to an extreme, “100% positivity all the time” can keep us trapped in some unhealthy habits and demotivate us to make important changes in our lives. This “good vibes only” approach often makes us avoid difficult emotions and replace it with a cheery, often (falsely) positive outlook. Research has actually shown that this “forced cheerfulness” has the opposite effect on our mood and well-being in the long-term.
Gratitude, on the other hand, is about recognizing those difficult emotions (pain, sadness, anger) and giving them the space to be looked at -- to be curious about why we are experiencing these emotions and what they may mean. (It doesn’t mean that these hard emotions take over our lives.) More research shows that “completing the cycle” of emotions (being curious and then finding a way to resolve them) is an important part of managing stress -- and gratitude plays a big part in this.
So…. gratitude ≠ positivity!
Now, you’re probably thinking: “That’s all well and good, but I’m so busy. I don’t have time to actively think about practicing gratitude.”
Well, my friend! I have some easy tips for you to get started.
Start small! Try focusing on the little, everyday things. Your health, for example. A pet or family member; your home or a hobby that you really enjoy.
Change your self-talk! Negative self-talk can have a big impact on your mental health. This is easier said than done, of course. But you gotta start somewhere!
Keep a gratitude journal. Think about setting aside 5 minutes in the evening to reflect on the day and list 3 things that you’re grateful for. Writing things down helps us really solidify things (instead of just being tossed around in our brains, mixed in with all the negativity and stress!).
Put post-it notes around the house of things that you’re grateful for. It never hurts to have a little reminder.
Say “Thank you!” to those around you. Your spouse or friend or even a co-worker. Thank them for being or doing something that has been your life a little bit easier ...or even just something you really appreciate about them.
For a fancier twist: try writing thank you notes (and no, not just after Christmas or your birthday. An out-of-the-blue thank you card can make someone’s day! And help you center yourself in your appreciation/love for them.
With this holiday season, take some time to practice your thankfulness. Hopefully, it will turn into a daily ritual that enriches your life, your health and your mentality!
<3 The Recharged Performance Therapy Team
References
https://www.pelvicsanity.com/post/2017/11/29/7-health-benefits-of-gratitude
https://www.pelvicsanity.com/post/2017/12/01/three-ways-to-cultivate-gratitude-throughout-the-year
https://gyngwinnett.com/blog/how-being-thankful-can-improve-your-health
https://www.npr.org/2020/06/02/867905101/want-to-be-happier-evidence-based-tricks-to-get-you-there
https://gyngwinnett.com/blog/how-does-stress-affect-gynecological-health
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3489271/
https://www.tandfonline.com/doi/figure/10.1080/02699931.2011.595393?scroll=top&needAccess=true&
https://www.psychologytoday.com/us/blog/the-high-functioning-hotspot/202107/what-is-toxic-positivity
Mommy Tummy- Diastasis Recti
Diastasis Recti is a condition normally seen at the end of pregnancy and after birth. It is normal until about 12 weeks postpartum. If you are still experiencing a “gap” after 12 weeks, you need to see a Pelvic Floor Physical Therapist for Diastasis Recti!
Good News- There is a Pelvic Floor Physical Therapist for you here in Melbourne, FL!
The #1 thing to do for your C-Birth Scar
Did you have a C-Birth (C-section)? If you did, or may have one in the future, then you NEED to read this latest installment to our Blog! We go over the easiest ways to help your scar heal and look better too! And schedule an appointment with pelvic floor physical therapy. You will thank us, we swear.
Cesarean Section
What does your posture look like?
Y’all- posture matters! You would be SHOCKED by how much better women FEEL & look when we get them in a better posture!
Watch this video from Dr. Paige! She goes over what “perfect” posture is and how to get your posture right! And schedule an appointment with pelvic floor physical therapy. You will thank us, we swear.
Diastasis Recti Muscles
Postpartum Recovery
In this blog, Dr. Paige goes over a few tips and tricks to improving recovery after delivery of your baby! You just went through a life changing event and should be cared for- even though most people don’t talk about recovering after birth. Learn how to better care for you so that you can better care for your baby! But more than anything- you need to go see a pelvic floor physical therapist! They will change your life!