The “latent” period of postpartum recovery occurs from 6 weeks to 6 months after delivery but full postpartum recovery takes up to 2 years (that we are aware of in 2025). By that time, your hair should stop falling out. You should no longer have physical symptoms (like bladder leakage or Diastasis Recti). Your period may come back around the 6 month mark, but it could take up to 2 years for your hormones to re-balance. If you’ve had a C-section, you may feel more tired at the 6 month mark than those who had a vaginal delivery. Mentally, you may be getting more into a routine as your baby is sleeping more. Though, of course, it is important to address any lingering mental health concerns.
Weeks 1-2 Postpartum
Here at Recharged PT, we’ve talked extensively about what to expect prior to getting pregnant as well as the 1st, 2nd, and 3rd trimesters. Heck, we’ve even done a deep dive on the fourth trimester. But, sometimes, it can be helpful to get back to basics: what your recovery may look like after you give birth. Having a general timeline for postpartum recovery can be helpful - here are the first two weeks laid out for you.
Ectopic Pregnancy
Gestational Diabetes
—> Hormones from the placenta block and diminish your body’s ability to use or make insulin. Insulin helps your body maintain the appropriate amount of glucose (blood sugar) in the blood. Weight gain and other factors make pregnant people more naturally insulin resistant – and some develop gestational diabetes as a result.
—> GDM does not develop because you had undiagnosed diabetes prior to pregnancy; it occurs because of the pregnancy. Usually diagnosed between 24 and 28 weeks, GDM can feel like a scary diagnosis.
Fortunately, GDM is a well-understood and well-managed diagnosis. We also have new information that came out in 2024 showing that GDM can be directly related to DAD’S HEALTH as his genetics are what determines the Placenta health.
Pregnancy Swelling!
We’re here today to talk about maybe one of the most common complaints seen during pregnancy and postpartum: swelling.
Swelling during pregnancy is usually pretty common in the lower extremities and feet. All the extra fluid that your body creates to help support a healthy baby can cause blood circulation to slow – and much of it accumulates in the legs and feet. Especially if you are up on your feet a lot!
Increasing Fertility
So! You’ve decided to take the leap into trying to conceive. As a very exciting (and sometimes nerve wracking!) time, a lot of things may feel overwhelming at first.
Here at Recharged PT, we’ve got all things pregnancy covered.
In the past, we have covered everything from what to expect each trimester to how to safely exercise and eat while pregnant. We have gotten into postpartum care and even the so-called “fourth trimester.” But another important factor to consider in your pregnancy journey is what to do before you get pregnant. Your lifestyle, mood and overall health can have a tremendous effect on your fertility and ability to conceive. And that is what we are here to talk about today. Aside from the mental, emotional, and relational dynamics involved in making this decision, your physical well-being is just as vital!
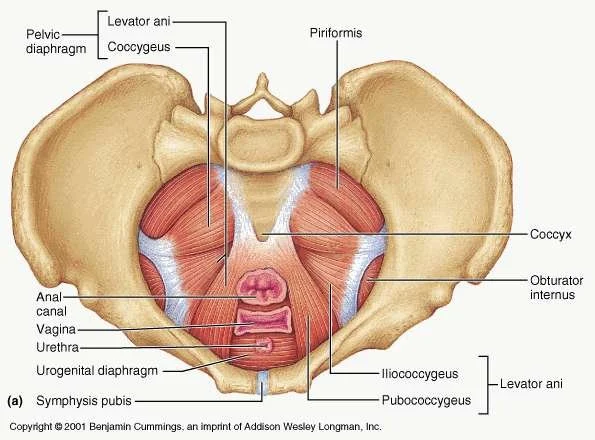
Bladder Prolapse
Cystocele (SIS-toe-seel) is when the bladder drops from its usual position and presses on the vaginal wall. A type of pelvic organ prolapse, cystocele or anterior vaginal prolapse, can occur if the pelvic floor muscles are weak, the organ is not in the correct spot in the pelvis in general (especially post child birth) or if there is too much pressure put on the pelvic floor. Common causes of a prolapsed bladder include repetitive stress over time (e.g., coughing, improper lifting) or during vaginal childbirth.
3rd Trimester Fun!
The final trimester is all about growth and preparation – for you and baby! This can be another physically and emotionally challenging time as you prepare for birth; balance feelings like excitement, fatigue, and worry; and experience physical discomfort as the baby grows. This is also generally the time that you take lactation and birth prep classes.
1st Trimester of Pregnancy
Overall, the first trimester of pregnancy is all about change and your growth: your body and your baby’s. It is also a time of variability in symptoms, emotions, and adjusting to a new stage of life. It is important to be gentle with yourself during this time and do things to keep yourself healthy, happy and whole!
After Surgery- Post Op
Today we are talking about how to care for yourself after you have surgery- this could be anything from a C-Section to a knee replacement. The info contained here isn’t super specific but that doesn’t make it any less important!!
Having surgery and recovering from it can be a very challenging process physically, mentally, and emotionally. Whether you elect to have it done or the procedure is absolutely vital to your health and well-being, surgery is trauma to your body: it takes a toll.
Birth Control- an overview
Today we want to talk about birth control (BC). There is a lot of information out there and it can definitely feel overwhelming to pick the type that is right for you, your body and your situation. And that is why we are here to help at Recharged PT! If you’re considering taking (or changing) birth control – commonly known as contraception – there are a variety of options available to you. Each one works a bit differently and comes with its own set of pros and cons. There is no “best” method of birth control.
The Skinny on Hormonal Health
Hormones are produced chemically by different glands throughout the body, such as your adrenal glands or sweat glands, to keep you as close to homeostasis as possible. This can include everything from the stress response with cortisol (which we’ve covered before) to hormones that affect digestion, temperature regulation, and mood. The pituitary gland, located deep in the brain, is the “puppet master” that controls the release of how much hormone and when to keep the body functioning.
Pelvic Health and Pelvic Floor Therapy in Melbourne, Florida. Dr. Paige, Dr. Laura, Dr. Sky
Pregnancy & Exercise
Overall, physical activity is highly encouraged for most pregnant women – particularly if you are low-risk. Everyone can benefit from exercise in some form within certain precautions. The most important part is that it feels good to you.
Pelvic Floor Physical Therapy, Melbourne, FL. Pelvic Health Rehab. Pregnancy. Pregnancy and Exercise
Kegels
There is a reason that Kegels are considered the classic pelvic floor exercise. They are very effective for a lot of pelvic floor issues — when done correctly for the right type of dysfunction. So before you start doing them, make sure they are the right exercises for you by chatting with a pelvic floor PT first.
Obturator Internus Pelvic Floor Pain
The Obturator Internus (OI) is a muscle that sits deep in the hip girdle, running from the front of the pubic bones and inserting onto the greater trochanter (the top bony part of the thigh bone). The OI is a deep hip stabilizer, which means it helps stabilize the head of the femur (thigh bone) to keep it in socket. This muscle is also responsible for external rotation – or rolling out– of the hip and thigh. Additionally, the OI shares a fascial connection to most, if not all, of the deep pelvic floor muscles. People with dysfunction of the Obturator Internus often complete of a deep groin, hip or back pain that won’t go away with regular stretching.
Pelvic Health, Pelvic Floor Rehab, Pelvic Floor Exercises, Pelvic Pain, Pain with Intercourse, Melbourne, FL, Postpartum, Postpartum Rehab, Pee Leakage, Dr. Paige, Dr. Laura, Recharged Performance Therapy
Urge Incontinence
Urge incontinence occurs when you have a sudden desire to go to the bathroom due a very quick and powerful bladder contraction. This is sometimes followed by the involuntary loss of urine before you can make it to a toilet. Urge incontinence (UI) is characterized by the need to go often throughout the day – especially at night (nocturia) – with small amounts of urine actually released. “Frequent” means more than 8x during the day and >2 at night. Enuresis (bed wetting) may also occur.
Pelvic Health, Pelvic Floor Rehab, Pelvic Floor Exercises, Urge Incontinence, Melbourne, FL, Postpartum, Postpartum Rehab, Pee Leakage, Dr. Paige, Dr. Laura, Recharged Performance Therapy
Dribbling After You Pee
Overflow Incontinence occurs when your bladder doesn’t completely empty when you go to the bathroom. You may or may feel the urge *to go* with this type of incontinence. But it is very common for only small amounts of urine to be released throughout the day as your bladder refills- which means you go to the bathroom all the time because you aren’t really emptying.
Stress Urinary Incontinence - Pee Leakage
One important thing to *note* here is that a lot of “Dr. Google” resources on SUI is that Kegels (tightening your PF muscles) will help with leakage by making the muscles stronger. But this is usually not the case!! The vast majority of people with pelvic floor dysfunction (and SUI) have have PF muscles that are too tight – NOT too loose. Because muscles need to be a certain length to work optimally, a muscle that is too loose OR too tight can be weak.